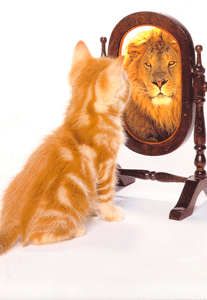
Fortunately, positive affirmations are almost as easy to define as they are to practice. Put simply, they are positive phrases or statements used to challenge negative or unhelpful thoughts.
Practicing positive affirmations can be extremely simple, and all you need to do is pick a phrase and repeat it to yourself.
You may choose to use positive affirmations to motivate yourself, encourage positive changes in your life, or boost your self-esteem. If you frequently find yourself getting caught up in negative self-talk, positive affirmations can be used to combat these often subconscious patterns and replace them with more adaptive narratives.
Science, yes. Magic, no. Positive affirmations require regular practice if you want to make lasting, long-term changes to the ways that you think and feel. The good news is that the practice and popularity of positive affirmations are based on widely accepted and well-established psychological theory.
One of the key psychological theories behind positive affirmations is self-affirmation theory(Steele, 1988). So, yes, there are empirical studies based on the idea that we can maintain our sense of self-integrity by telling ourselves (or affirming) what we believe in positive ways.
Very briefly, self-integrity relates to our global self-efficacy—our perceived ability to control moral outcomes and respond flexibly when our self-concept is threatened (Cohen & Sherman, 2014). So, we as humans are motivated to protect ourselves from these threats by maintaining our self-integrity.
Self-affirmation theory has three key ideas underpinning it. They are worth having in mind if we are to understand how positive affirmations work according to the theory.
First, through self-affirmation, we keep up a global narrative about ourselves. In this narrative, we are flexible, moral, and capable of adapting to different circumstances. This makes up our self-identity (Cohen & Sherman, 2014).
Self-identity (which we’re seeking to maintain, as mentioned before) is not the same as having a rigid and strictly defined self-concept. Instead of viewing ourselves in one “fixed” way, say as a “student” or a “son”, our self-identity can be flexible. We can see ourselves as adopting a range of different identities and roles. This means we can define success in different ways, too.
Why is this a good thing? Because it means we can view different aspects of ourselves as being positive and can adapt to different situations much better (Aronson, 1969).
Secondly, self-affirmation theory argues that maintaining self-identity is not about being exceptional, perfect, or excellent (Cohen & Sherman, 2014). Rather, we just need to be competent and adequate in different areas that we personally value in order to be moral, flexible, and good (Steele, 1988).
Lastly, we maintain self-integrity by acting in ways that authentically merit acknowledgment and praise. In terms of positive affirmations, we don’t say something like “I am a responsible godmother” because we want to receive that praise. We say it because we want to deservethat praise for acting in ways that are consistent with that particular personal value.
The development of self-affirmation theory has led to neuroscientific research aimed at investigating whether we can see any changes in the brain when we self-affirm in positive ways.
There is MRI evidence suggesting that certain neural pathways are increased when people practice self-affirmation tasks (Cascio et al., 2016). If you want to be super specific, the ventromedial prefrontal cortex—involved in positive valuation and self-related information processing—becomes more active when we consider our personal values (Falk et al., 2015; Cascio et al., 2016).
The results of a study by Falk and colleagues suggest that when we choose to practice positive affirmations, we’re better able to view “otherwise-threatening information as more self-relevant and valuable” (2015: 1979). As we’ll see in a moment, this can have several benefits because it relates to how we process information about ourselves.
Now that we know more about the theories supporting positive affirmations, here are six examples of evidence from empirical studies that suggest that positive self-affirmation practices can be beneficial:
If you’re interested in finding out more about the proven benefits of practicing positive affirmations, this article by Critcher and Dunning (2015) is worth a read. The article looks at the ways in which practicing affirmations has been shown to foster a broader sense of self-concept.
As the studies above suggest, positive affirmations can help us to respond in a less defensive and resistant way when we’re presented with threats. One study that was mentioned above showed that smokers reacted less dismissively to graphic cigarette packet warnings and reported intention to change their behavior (Harris et al., 2007).
But more generally, an adaptive, broad sense of self makes us more resilient to difficulties when they arise. Whether it’s social pressures, health information that makes us feel uncomfortable, or feelings of exclusion, a broader self-concept can be an extremely helpful thing to have.
As inherently positive statements, affirmations are designed to encourage an optimistic mindset. And optimism in itself is a powerful thing. In terms of reducing negative thoughts, affirmations have been shown to help with the tendency to linger on negative experiences (Wiesenfeld et al., 2001).
When we are able to deal with negative messages and replace them with positive statements, we can construct more adaptive, hopeful narratives about who we are and what we can accomplish.
This kind of affirmation is a positive statement about your physical well-being. Popularized by author and speaker Louise Hay, these affirmations are based on the idea that your thoughts can influence your health for the better. You don’t have to be unwell to practice healing affirmations; this idea can be just as helpful for healing emotional pain if you find the idea rings with you.
Examples from Hay’s website include:
“My happy thoughts help create my healthy body,”
and
“Wellness is the natural state of my body. I am in perfect health.”
This definition is still a little ambiguous so to elaborate, basically positive affirmations, what most people mean by them are positive phrases which you repeat to yourself which describe how you want to be.
The theory (we believe it is much more than just a theory!) is that when you first start saying your positive affirmations, they may not be true, but with repetition they sink into your subconscious mind, you really start to believe them, and eventually they become your reality, they become a self fulfilling prophecy and actually become true.
Over time they overwrite any limiting or negative beliefs you may have about yourself or about not being able to do something, and replace them with positive thoughts and beliefs which instill confidence, belief, positivity, ambition and much more.
It is perhaps easier to see in a real life example:
 I am confident
I am confident* these affirmations are taken from across our affirmations for confidence range.
Someone who is perhaps a little shy or un-confident would repeat these affirmations. They would want to change themselves from being shy and introverted to becoming self confident and more outgoing perhaps, and so they would
use positive affirmations and repeat them over and over.. and eventually they would start to sink in – the repetitive, positive self talk would start to become a self fulfilling prophecy.. Well in just the same way (but reversed) you can use the power of positive repetition for yourself!
Using positive affirmations gives you back control of your mind and the information it receives. It puts you in the driver’s seat of your mind and lets you flood it with positive information which will change you for the better!
We hope you have enjoyed this simple introduction to positive affirmations, you can learn more in our series of articles designed to get you started – next in the series is our full free guide to using positive affirmations, or you can begin straight away – choose your area of development and pick your affirmations using the categories to the right.
Everything you need to know about symptoms, treatments, risk factors, and relapses so that living with bipolar depression is a little more manageable.
Article by:
Rebecca Dolgin
Whether you’ve just been diagnosed with bipolar depression, suspect you may have it, or someone in your family has it, you may be wondering what the next steps are and what this label really means. We’ve talked to the experts, read the research, and listened to people who have bipolar describe what it’s really like. Here, we’re going to share with you everything we’ve learned along the way including an as-told-to story from a couple facing the challenges of bipolar disorder and how they deal, a report on new treatments, and a piece describing what the symptoms feel like dispelling the common misconceptions.
Let’s start with what it means to have a bipolar disorder diagnosis. Bipolar disorder is a condition that essentially hijacks your moods. (We’ll get more into how in a sec.) Just under 3 percent of the U.S. population has bipolar, though many of those people (up to 40 percent) were first diagnosed with depression. That’s because people who have bipolar disorder experience a lot of the same symptoms as those who are depressed. The difference is, when you have bipolar, you’ll also have episodes of mania (sometimes called hypomania, if it’s less extreme). Because the manic episodes are the key distinguishing factor from regular depression, up until recently, bipolar disorder was referred to as manic depression.
Types Of Bipolar
Not all bipolar is the same. There are three types:
Bipolar I: Periods of severe mood episodes from mania to depression, which may require hospitalization.
Bipolar II: Periods of less severe mood episodes from a milder form of mood elevation, involving episodes of hypomania that alternate with periods of depression.
Cyclothymic disorder: Moods cycle between brief periods of hypomanic symptoms and brief periods of depressive symptoms. Neither are as extreme or long-lasting as with Bipolar I or Bipolar II.
Symptoms of Bipolar
Bipolar is almost like two diseases in one. To be diagnosed you need to have both manic symptoms and depressive ones. But, even still, the depressive symptoms are far more frequent than the manic ones. For those who have bipolar I, the depressive symptoms outpace the manic ones 3:1. And, for bipolar II, there are even more depressive episodes—it’s 40:1. This explains why so many people with bipolar are misdiagnosed with depression at first.
Depressive symptoms related to bipolar are may include:
Low energy
Low motivation
Loss of interest
Sadness
Feeling empty
Hopelessness
Significant weight loss
Fatigue
Indecisiveness
Inability to concentrate
Insomnia
Manic symptoms related to bipolar may include:
Abnormally upbeat
Euphoric
Jumpy
Wired
Racing thoughts
Pressured speech
Abnormally talkative, sometimes jumping from topic to topic
Feeling like you don’t need as much sleep
Poor decision-making and risk-taking
Being easily distracted
Irritable or impatient
Overly self-confident, feeling grandiose
Why Bipolar Is Tricky To Diagnose
Bipolar disorder may go unrecognized for up to a decade. Misdiagnosing it as depression is part of the reason. But the fact that there isn’t a single, definitive test that says, “yep, you have bipolar” also contributes to it slipping through the cracks. Doctors have to rely on how their patients describe the way they’re feeling. (Or how their loved ones describe it.)
This isn’t to say it’s arbitrary. There is a screening called the Mood Disorders Questionnaire (MDQ), which was developed to assesses lifetime history of mania and hypomania. It’s a simple checklist of 13 symptoms and a couple of questions about timing and severity.
Like with other disorders, psychiatrists and researchers are starting to recognize that bipolar can be thought of as a spectrum, not just a series of symptoms where you either check the box or you don’t. Different people can experience bipolar in very different ways, whether that means the ratio of depressive cycles to manic ones, having mixed episodes (where you feel both euphoric and down), or the ways the symptoms manifest. For some people, pressured speech may be the giveaway of a manic phase, for another it may be risky behavior.
Suicide Risk And Bipolar
One of the biggest concerns with bipolar is suicide. The numbers are pretty astounding: Someone with bipolar has a 30 percent chance of attempting suicide over the course of their lives. There’s been some debate over if the risk is higher for bipolar I, but most of the research shows it’s about the same for both bipolar I and bipolar II. One aspect of bipolar that does seem to increase suicide risk is having “mixed-features specifier,” where you feel the highs and lows at the same time.
If you have bipolar or someone you love has bipolar, get help if you notice the following:
Feeling more depressed than usual
Lack of interest in activities once enjoyed
Anger
Shame or humiliation
Mood swings
Talking about suicide or saying their lives have no purpose
Feeling like a burden or stuck
Isolating from others
Giving away possessions or writing a will
Driving recklessly
For a full list of signs and how to help, click here.
Bipolar Differences in Men and Women
For the most part, men and women have the same symptoms, and one gender isn’t more likely to have bipolar. Still, there are some distinct differences. One example is women with bipolar are three times more likely to get migraines than men. They’re also more likely to have depressive episodes and have more rapid cycling. Click here to read more about the gender differences.
Risk Factors for Bipolar
Genetics are a big factor. Having a sibling or parent with the disorder ups your chances, but it’s not the only indicator. Traumatic events and drug or alcohol use may also contribute. Some new research shows that people with bipolar may have slightly different brain structures (see below). There’s also a connection between pregnancy and bipolar. It seems that pregnancy and the act of giving birth can trigger postpartum bipolar disorder in some women. And, between 50 percent and 70 percent of women with bipolar disorder will experience a recurrence after a new baby, according to findings in the American Journal of Psychiatry.
Bipolar Treatments
Bipolar is a chronic mental illness but it doesn’t have to dominate your life. Medication can level out your moods. And, since everyone responds differently to medications it can be a bit of trial and error before you find the right one. Generally, there are three types of medication:
Anti-psychotics These are usually prescribed right away because they work immediately, but they’re not necessarily going to be the long-term treatment plan.
Mood stabilizers This category includes medicine like lithium, which has the strongest evidence of long-term benefits.
Anti-depressants These are somewhat controversial for two reasons: they focus just on the depressive episodes and some research has found they’re no more effective than a placebo.
Non-prescription therapy is also really important, including family therapy. It helps everyone understand what’s happening and why. There are also lifestyle changes that make a big impact:
Getting regular sleep. Not getting enough sleep can set off a manic episode, but any kind of disrupted sleep routines should be a flashing warning light that you might be about to go into either a depressive or manic episode.
Eating well. There is a lot of research on how food can affect your mood.
Managing stress. Stress can be a trigger, so it’s helpful to have tools like meditating or practicing yoga.
Sticking to a routine: Taking your meds on a regular schedule, going to therapy, and trying to keep your days as predictable as possible will help keep your mood in check.
In addition, there are some newer complementary therapies being researched that are showing major promise, some could even help patients decrease their medication doses. Click here to read about them.
Bipolar Relapses
Part of the frustration for people with bipolar is the relapse rate. You can be doing everything right, taking your medication, going to therapy, exercising, and still the conservative estimates that you’ll have a relapse are 73 percent within five years. To decrease your odds, take your medicine, avoid triggers, chart your moods (try apps like Daylio or Mod Tracker), and do something as soon as you notice a major mood shift. It’s much easier to get back on course if you get help early.
People With Bipolar May Also Have
If you have bipolar, you’re also more likely to abuse drugs and alcohol. This could be the result of self-medicating or the effect of big risk-taking during the euphoric phase. There are a cluster of other psychiatric illnesses that often go along with bipolar: 21 percent of people with bipolar also have panic disorder and 21 percent also have obsessive-compulsive disorder.
Your Brain on Bipolar
Intuitively it seems like there has to be something different about the bipolar brain. And, it turns out, there is. Magnetic resonance imaging has shown what scientists call a reduction of critical thickness in the ventrolateral prefrontal cortex. This is the area of the brain that assesses risk and could explain why people with bipolar don’t process dangerous situations the same way. The left side of the amygdala (see that little yellow dot, below), is kind of like the command central of emotion regulation, and it’s less active in someone with bipolar. A third distinction between normal and bipolar brains came from a study out of Canada. The research team found that in people with bipolar disorder, certain parts of the hippocampus are smaller than they are in both people with major depressive disorder and in people without mood disorders. And, they didn’t stop there, they found that the reductions in size were most severe among patients with bipolar I disorder.
conflict
Present Tense Affirmations
I am in control
I always listen to my conscience
I make healthy and positive decisions
My mind is at peace with itself
I am strong against temptation
I always take the action that I know is right
I make decisions and follow through
I always make the choice that is best for my future
My decisions and actions are always aligned with my long term goals
I have strong discipline and always stick to my intentions
Future Tense Affirmations
I will resolve my inner conflicts
I will always listen to my conscience
Harmony is developing between my actions and my intentions
I am changing into someone who always makes the right choice
I am finding it easier to do what I know I should
My discipline is getting stronger
I will become someone who stays focused even when tempted by distraction
Making plans and sticking to them is starting to feel easier
I will set goals for myself and stay focused on taking action to achieve them
I am transforming into someone who is always on the path to success
Natural Affirmations
I find it easy to do what I know is best
Following through on my intentions comes naturally to me
I am naturally focused on reaching my goals
My conscience is my one true guide
There is natural harmony between my goals and my actions
Resisting distractions is something I just naturally do
It is normal for me to make choices that align with my long term interests
Resolving inner conflict is the key to succeeding in every area of my life
Choosing the healthiest course of action is easy for me
Others see me as someone who can make a firm decision and stick to it
help
Present Tense Affirmations
I am improving myself
I have the power to change
I always take care of myself
I am a positive thinker
I have the confidence to succeed
I am happy with myself
I am constantly growing and developing
I am taking steps to better my life
I believe in myself
I love and respect myself deeply
Future Tense Affirmations
My life is beginning to improve
I will always nurture myself
My attitude is becoming more positive
I will keep making progress
I will love and accept myself unconditionally
Having confidence in myself is becoming easier with each passing day
My self-belief is growing
I am starting to make positive changes in my life
I am transforming into someone who lives a healthy and balanced life
Everyday I become more empowered to take control of my life
Natural Affirmations
Positive thinking comes naturally to me
I have the desire to be healthy and happy
It is easy for me to make lasting positive changes
Personal growth is an important part of my life
I am a naturally balanced and healthy person
I have complete confidence in myself
I enjoy improving myself and bettering my life
I deserve to live a great life
Believing in myself is my normal state of mind
I have the power to create the life of my dreams
Develop courage
Present Tense Affirmations
I am courageous
I am brave
I am fearless
I always stand up for myself
I am developing courage
I am ready for anything that comes my way
I am strong and full of courage
I push through my fear and do it anyway
I am courageous when others are scared
My courage helps to inspire others
Future Tense Affirmations
I will develop courage
I will smash through fear and rise to the occasion
I am becoming more courageous with each passing day
I will transform into a strong and fearless person
Fearlessness is developing within me
Each day I feel stronger and more courageous
Others will notice my fearlessness
I will always stand up for what I believe in
I will speak up for myself
I am becoming more daring and adventurous
Natural Affirmations
I am naturally courageous
Courage comes easily to me
I always find a way to call forth courage when I need it
I am the kind of person who feels fear but does it anyway
Being brave comes naturally to me
Developing courage is something I just know I can do
Being strong in the face of adversity is one of my best traits
Others look to me for leadership at difficult times
Standing up for myself is something I just naturally do
It is important that I become a courageous person
Present Tense Affirmations
I am free from my past regrets
I am living my life without regrets
I am at peace with my past regrets
My mind is focused on enjoying the present moment
I am on the path to a brighter future
I accept my life and everything I have done
I live in the present and look to the future
I am letting go of my past regrets
I am always positive even when remembering my past regrets
I accept my past regrets knowing they have made me a better person
Future Tense Affirmations
I will live without regrets
My enthusiasm for life is growing
I am starting to live life to the max
Accepting my past becomes easier with each passing day
I am transforming into someone who lives happily in the present moment
Letting go of my regrets is becoming easier and more natural
I will move on with my life
I will become free from regrets
I am starting to see that my future will be bright and happy
I am beginning to see my past in a more positive light
Natural Affirmations
I deserve to live a live without regrets
I find it easy to live without regrets
Living my life free from regrets comes naturally to me
I have accepted my past regrets and am now ready for the future
It will feel incredible to free myself from past regrets
I am moving forward and leaving my regrets in the past
I have hope for a brighter future
Living a life free from regrets will make me happy and content
I have accepted my regrets and am ready to move on
My mind is relaxed and focused on the present moment
Self confidence
Present Tense Affirmations
I always succeed
I am confident
I achieve massive success
I am capable of reaching any goal
I am ready for anything
I am always positive
My mind is completely focused on success
I am able to handle whatever life brings my way
I am a beautiful person
Others see me as confident and successful
Future Tense Affirmations
I will believe in myself
I will develop an unshakeable self belief
Each day I feel more powerful and capable
I am transforming into someone who can achieve anything
I will achieve whatever I set my mind to
I am starting to feel more and more confident in my abilities
I will always love, respect, and believe in myself unconditionally
Self belief is transforming me into a highly successful person
Others are beginning to notice my confident attitude
Developing self belief will help me to achieve my goals
Natural Affirmations
I believe in myself completely
Achieving success is normal for me
Self belief comes naturally to me
I believe that I can achieve anything I want
Others see me as a highly capable person
I am the kind of person who confidently goes after success
It is normal for me to feel great about myself
I find it easy to pursue my goals with confidence
I am a high achiever
I always find a way to succeed